Long term changes of posterior corneal elevation after myopic laser in situ keratomileusis
阅读量:818
DOI:doi: 10.3978/j.issn.1000-4432.2016.03.07
发布日期:2024-11-27
作者:
Honghe Xia ,Riping Zhang ,Alvin L. Young ,Mingzhi Zhang
展开更多 '%20fill='white'%20fill-opacity='0.01'/%3e%3cmask%20id='mask0_3477_29692'%20style='mask-type:luminance'%20maskUnits='userSpaceOnUse'%20x='0'%20y='0'%20width='16'%20height='16'%3e%3crect%20id='&%23232;&%23146;&%23153;&%23231;&%23137;&%23136;_2'%20x='16'%20width='16'%20height='16'%20transform='rotate(90%2016%200)'%20fill='white'/%3e%3c/mask%3e%3cg%20mask='url(%23mask0_3477_29692)'%3e%3cpath%20id='&%23232;&%23183;&%23175;&%23229;&%23190;&%23132;'%20d='M14%205L8%2011L2%205'%20stroke='%23333333'%20stroke-width='1.5'%20stroke-linecap='round'%20stroke-linejoin='round'/%3e%3c/g%3e%3c/g%3e%3c/svg%3e)
关键词
Posterior corneal elevation (PCE)
myopia
laser in situ keratomileusis (LASIK)
cornea
摘要
Background: Corneal ectasia is a serious complication after laser in situ keratomileusis (LASIK). Ideally,
patients at risk of ectasia should be identified prior to laser as unsuitable for LASIK, however, at present,
there is no absolute test, system, or marker that can unequivocally identify patients at risk of developing
ectasia. It has been suggested that changes in the forward protrusion of the posterior cornea or posterior
corneal elevation (PCE) may be a key to the early detection of ectasia after LASIK. The purpose of this study
was to examine the long term changes of the PCE after myopic LASIK using the ORBSCAN®
IIz (Bausch &
Lomb, Rochester, USA) and to evaluate the contributory preoperative factors to PCE changes.
Methods: This was a retrospective longitudinal case series. Forty-two eyes of 23 consecutive myopic
patients who underwent uneventful LASIK surgery 6 years ago were recalled for a postoperative follow-up
examination using the ORBSCAN®
IIz to determine the elevation changes to the posterior corneal surface
from the preoperative measurements. A forward shift of the posterior surface was given a negative value.
Correlation analyses and forward stepwise regression analyses were performed to evaluate the effect of each
of the preoperative parameters on the changes in PCE. Statistical and graphical analyses were performed.
Results: There was no statistical difference between the mean best-fit sphere (BFS) pre-LASIK and 6 years
postop (P=0.25). Forty-two post-LASIK eyes had a mean posterior displacement of -9.38±9.84 μm (range,
12 to -31 μm) 6 years after LASIK. Forward stepwise multiple linear regression analysis indicated that the
ablation spherical equivalent (ASE) was the only indicator of the forward shift of the posterior cornea after
LASIK.
Conclusions: The present study identified a significant forward shift of the posterior cornea 6 years after
LASIK. The ASE was the most significant prognostic determinant for forward protrusion of the posterior
cornea after LASIK.
全文
Introduction
Laser in situ keratomileusis (LASIK) has been a wellrecognized
procedure for the correction of myopia.
However, LASIK can weaken the underlying stroma and
may lead to an increased risk for postoperative keratectasia(1-3). Corneal ectasia is a serious complication after LASIK,
resulting in an increase in myopia and astigmatism and the
loss of visual acuity due to progressive corneal steepening.
The onset of ectasia may be early or delayed of up to more
than a year after surgery(2-5). The incidence of keratectasia after myopic LASIK has been estimated to be 0.04% to
0.6%(2,3,6).
Although posterior corneal elevation (PCE) change
consistent with progressive ectasia may be observed as
early as 4 to 6 weeks after LASIK, post-LASIK ectasia is
usually diagnosed 13 months after surgery(5). Martin et al.
reported a PCE trend that increased in the first month
after LASIK and reduced with time, without any significant
differences 1 year after LASIK(7). Few other studies have
described the PCE more than 1 year after LASIK, with the
longest reported follow-up period of 18 months (8). Longer
term results are important, as keratectasia can occur 6 to
20 months after LASIK(1,4,5).
The purpose of this study was to examine the long term
changes (6 years postop) of the PCE after myopic LASIK
using the ORBSCAN®
IIz and to evaluate the contributory
preoperative factors to PCE changes.
Methods
This was a retrospective longitudinal case series. Written
informed consent was obtained from each participant. The
study adhered to the tenets of Declaration of Helsinki, and
was approved by the Institutional Review Board of the Joint
Shantou International Eye Center (JSIEC). The inclusion
criteria were: (I) myopia of≥−1.00DS before LASIK; (II) no
contraindications to LASIK (such as Forme Fruste
Keratoconus, dry eyes); (III) uneventful LASIK procedures;
(IV) a minimum postoperative follow up of 6 years.
One hundred and sixteen consecutive subjects were
recalled by phone for a postoperative examination in 2012. Twenty-three subjects with a total of 42 eyes returned for
the visit, while 93 subjects (177 eyes) failed to attend.
There were no marked differences between subjects who
attended and those who were unavailable for the followup
examination with respect to age, gender, preoperative
SE, central corneal thickness (CCT), preoperative PCE &
preoperative intraocular pressure (IOP) (Table 1).
Table 1 Characteristics of subjects who attended in comparison to those who were unavailable for the long term postoperative examination
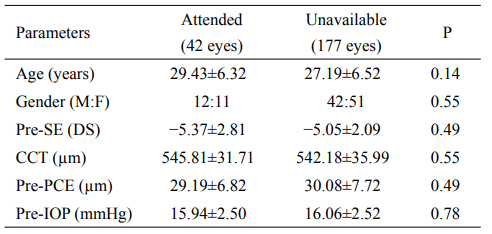
pre-SE, preoperative spherical equivalent; CCT, central
corneal thickness; pre-PCE, preoperative posterior corneal
elevation; pre-IOP, preoperative intraocular pressure
All LASIK procedures were performed with the
Technolas217z100 laser (Bausch & Lomb, Rochester, USA)
by four trained ophthalmologists at the JSIEC. All the
surgeons adopted the same standard procedure, consisting
of the application of a narrow beam, flying-spot excimer
laser with eye tracking assistance (Technolas217z100,
Bausch & Lomb, USA). The Technolas217z100 laser has an
emission wavelength of 193 nm, a fixed pulse repetition rate
of 50Hz and a radiance exposure of 120 mJ/cm2
. Suction
rings of 8.5 or 9.0 mm in diameter were used and LASIK
flaps were cut by the Hansatome Microkeratome (Bausch &
Lomb, Rochester, USA) with a target thickness of 160 μm.
ORBSCAN® IIz (Bausch & Lomb, Rochester, USA,
version 3.12) was used to image the corneas of all the patients
preoperatively, 1-month postop and at the 6-year followup
visits. The system and software were identical. The
changes of the posterior corneal surface were determined
by the ORBSCAN®
IIz posterior best-fit sphere (BFS). The
PCE was defined as the value relative to the BFS of a single
map and was used to compare the pre-operative and postoperative
posterior corneal surface changes(9).
The difference in elevation was considered to be the
displacement of the posterior corneal surface. Changes in
the posterior surface were determined by subtracting the
postoperative elevation data from the preoperative data
based on the maximal differences. A forward shift of the
posterior surface would result in a negative number.
Corneal thickness was measured by the IOPac®
advanced
ultrasonic pachymetry (Heidelberg Engineering, Germany),
with the lowest CCT reading taken to be the thinnest part
of the cornea.
Residual bed thickness (RBT) was calculated by using the
thinnest CCT reading and subtracting the non-nomogram–
adjusted ablation depth and the flap thickness of 160 mm.
Statistical analysis
All analyses were performed using statistical software
(StatLab, SPSS for windows, version 13.0; SPSS, Inc.,
Chicago, Illinois, USA). Paired-sample t test was used for the analysis of PCE and BFS. Pearson correlation
analysis was used to assess the effect of each of preoperative
parameters on PCE changes. Stepwise forward multivariate
linear regression analyses were used to evaluate the
contributory preoperative factors to PCE changes. All
continuous variables are presented as mean±standard
deviation. A P value of <0.05 was considered as statistically
significant.
Results
In 42 eyes, only 32 eyes had 1 month postoperative data.
The posterior BFS of the 32 eyes for the preoperative,
1-month and 6-year visits were as follows (Figure 1):
6.40±0.19 mm (range, 6.09–6.70 mm); 6.27±0.19 mm (range,
5.95–6.7 mm) and 6.41±0.20 mm (range, 6.07–6.68 mm)
respectively. The mean differences between the BFS preLASIK
and 1 month postop were found to be statistically
significant (P<0.01). However, there was no statistical
difference between the mean BFS pre-LASIK and 6 years
postop (P=0.25).
There were statistically significant differences identified
in the PCE (P<0.01) between the pre-LASIK, 1-month and
6-year postop visits: at 30.00±6.90 μm (range, 10–45μm),
58.53±12.79 μm (range, 35–85μm) and 38.97±9.50 μm
(range, 18–60μm) respectively. Figure 2 illustrates the PCE
evolution of the 32 eyes over the course of time.
Forty-two eyes were examined with the ORBSCAN®
IIz for the study. The M:F ratio was 12:11. Four patients
had LASIK performed in 1 eye only. The mean age was
29.43±6.32 years (range, 18–39 years). Data at the time of
the preoperative examination were showed in Table 2.
The minimum RBT was set at 250 μm, but 1 patient in
the study ended up with a computed residual thickness of
245 μm. The posterior BFS of the 42 eyes changed from
6.39±0.21 mm (range, 6.09–6.90 mm) before surgery to
6.39±0.23 mm (range, 6.00–6.91 mm) at 6 years postop. The
differences were not statistically significant (P=0.64).
The mean PCE in the 42 eyes was 29.19±6.82 μm (10–45 μm) before LASIK and 38.57±9.10 μm (range, 18–60 μm)
6 years after LASIK. The difference was statistically
significant (P<0.01). The mean change in PCE 6 years after
LASIK was−9.38±9.84 μm (range, 12 to-31 μm).
Pearson correlation analysis for PCE change at 6 years after LASIK is illustrated in Table 3.
The preoperative parameters included preoperative SE,
ASE, central ablation depth, CCT, IOP and RBT. The RBT, preoperative SE and ASE were positively correlated
with the PCE changes and the central ablation depth was
negatively correlated with the PCE changes at 6 years
postop. Forward stepwise regression analysis revealed
that the ASE was the only contributory preoperative
factor (P=0.005), suggesting that higher ASE values were
associated with a greater forward shift of the PCE (Figure 3).
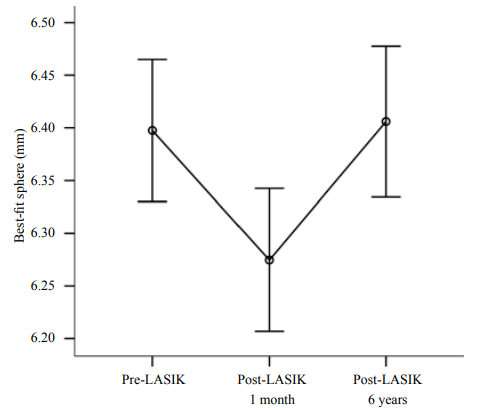
Figure 1 Best-fit sphere evolution at each visit of 32 eyes. Bars represent the 95% confi dence interval.
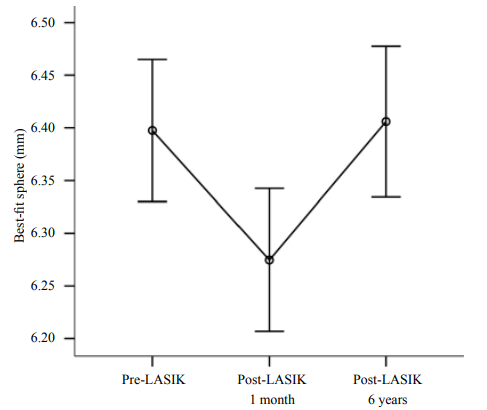
Figure 2 Posterior corneal elevationt evolution at each visit of 32 eyes. Bars represent the 95% confi dence interval.
Table 2 Data at the time of the preoperative examination (n=42 eyes)
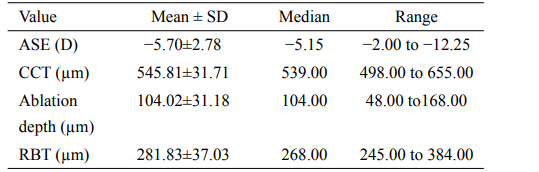
ASE, ablation spherical equivalent; CCT, central corneal
thickness; RBT, residual bed thickness.
Table 3 Correlation analysis and stepwise forward regression analysis for preoperative factors on the posterior corneal elevation (PCE) changes 6 years after LASIK
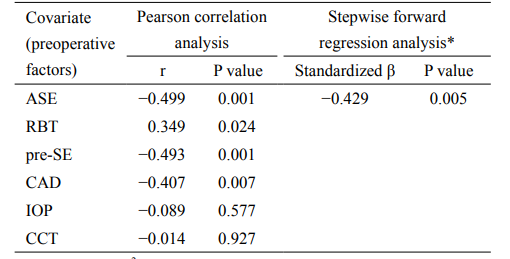
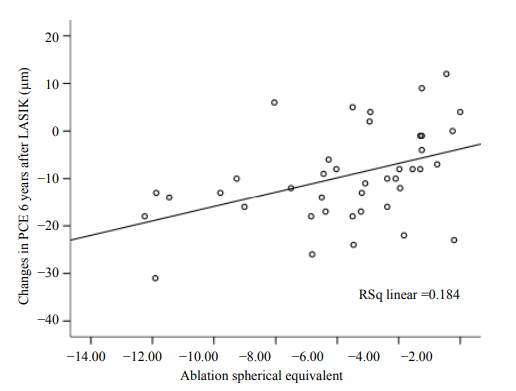
Figure 3 Scatterplot diagram showing the correlation between the
ablation spherical equivalent and the posterior corneal elevation
changes at 6 years postop. Ablation spherical equivalent values
were positively correlated with the PCE changes, suggesting that
higher ablation spherical equivalent values were associated with a
greater forward shift of posterior corneal elevation. PCE, posterior
corneal elevation.
Discussion
Reported risk factors for post LASIK corneal ectasia
include high myopia, low residual stromal bed thickness,
topographical abnormality such as Forme Fruste
Keratoconus, and multiple LASIK procedures(4). Ideally,
patients at risk of ectasia should be identified prior to laser
as unsuitable for LASIK; however, at present, there is no
absolute test, system, or marker that can unequivocally
identify patients at risk of developing ectasia. It has been
suggested that changes in the forward protrusion of the
posterior cornea or PCE may be a key to the early detection
of ectasia after LASIK(7). Another advantage of focusing
on the posterior surface of the cornea is that the PCE map
is not influenced by tear film irregularities or the use of
artificial tears(10).
Based on the results identified from the three visits of
the 32 eyes, we noted a trend towards PCE that increased
in the first month after LASIK and reduced with time,
with significant differences present even at 6 years post
LASIK. The exact magnitude of displacement predisposing
to ectatic changes is however not known. The posterior
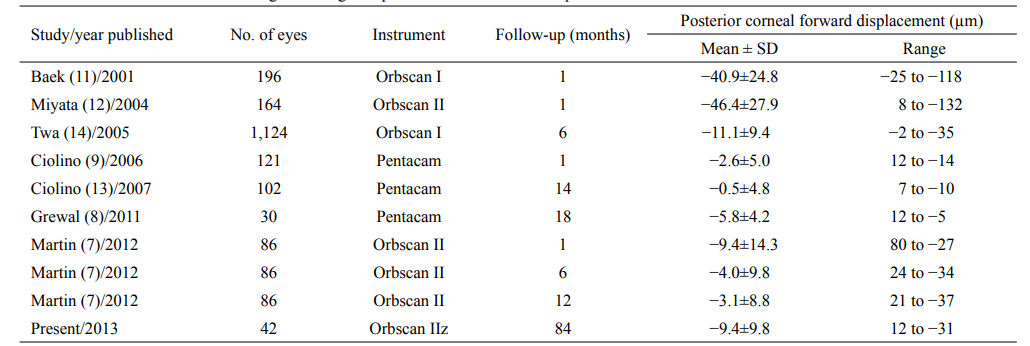
corneal displacement in the 42 eyes found in this study was−9.38±9.84μm (range, +12 to−31 μm), which was similar to
previously reported studies with the Orbscan(8-14)(Table 4).
Nobody included in the study had serious corneal ectasia or
keratoconus. It suggests that the average elevation change
observed here at 6 years means good corneal stability.
Martin et al.(7)described that an estimated RBT greater
than 300μm will be free from any significant posterior
forward shift (P=0.05 and R2
=0.002, P<0.86). Patients
with an estimated RBT less than 300μm had a significant
posterior forward shift in the first month after LASIK
(P<0.05), but this difference was not significant at 1 year
after surgery (P>0.05). Although the RBT has been shown
to influence the PCE(14,15), it was not significantly
associated with the PCE changes in our long term follow
up study. In our study, the mean RBT was 281.83±37.03 μm
(range, 245–384 μm), and multivariate linear regression analyses revealed that the ASE was the only indicator of the
forward shift of the posterior cornea after LASIK (P=0.001),
suggesting that higher ASE values were associated with
a greater forward shift of the PCE. Pearson correlation
analysis showed that the ablation depth, preoperative SE
and RBT were also significantly associated with PCE
changes. This may be partially related to the correlation
of the ASE with the ablation depth, preoperative SE and
RBT (r=0.818, P=0.000; r=0.992, P=0.000, and r=−0.540, P=0.000, respectively). In other words, patients with a
higher preoperative SE receive a greater ablation depth, a
higher ASE values and a thinner RBT left. This is likely the
reason that the forward stepwise regression analysis did not
include these covariants in the final models.
In our study, the ORBSCAN® IIz documented larger
changes in the PCE after LASIK than the changes reported
by Ciolino(13)and Grewal(8)using the Pentacam (Oculus
Optikgeräte GmbH, Wetzlar, Germany). One explanation
for this observation is the difference in technology used
to measure the cornea. Although the ORBSCAN® IIz
topographer is better than previous technology used to image
the cornea, the use of the Orbscan to assess post-LASIK
PCE may still be controversial as the accuracy of the Orbscan
in assessing the posterior corneal surface remains a subject of
debate(14,16). The Orbscan’s mathematical reconstruction of
the posterior cornea may lead it an overestimation of the PCE
above the BFS (17). Furthermore, Herna’ndez-Quintela (18) and Maloney (19) suggested that the variability between
pre-LASIK and post-LASIK PCE Orbscan measurements
may be a source of artificially observed ectasia. Different
hypotheses have been proposed to explain the problems with
the Orbscan in assessing the posterior corneal curvature after
LASIK (20). The effect of eyelids, eyelashes and reflections
could provide an incomplete map, especially in the periphery
of the cornea. If the peripheral data are missing, the elevation
maps could be affected (21).
Posterior ectasia typically presents approximately 13 months after LASIK (6), our long term follow-up (6 years) study provides more evidence on the stability of the posterior cornea post LASIK. To the best our knowledge, this is the longest follow up study on the PCE changes after LASIK.
There are several limitations in this study. Although this cohort of patient was retrospectively identified and invited back for an updated examination, there was a high loss to follow-up rate (80%) and we ended up with a relatively small number of patients (only 42 eyes). On the other hand, additional data from the period between 1 month post LASIK to 6 years postop would be highly desirable, thus we would not be able to identify if there were any changes in between and the time when these changes in the posterior elevation may have taken place or stabilized. The adjusted R2 value of the final regression model for the changes in PCE was 0.184, indicating a significant degree of variation in the dependent variables of the changes in PCE 6 years post LASIK. Furthermore, the changes in PCE are only one of the outcomes used for assessing keratectasia after LASIK. Another useful parameter would be corneal topography. Other parameters, such as the ablation depth and RBT may also be considered when evaluating keratectasia after LASIK. Therefore, the changes in PCE after LASIK must be interpreted in the light of above variables.
Table 4 Results of studies evaluating the changes in posterior corneal elevation post LASIK
Conclusions
In conclusion, the present study identified a significant
change in the PCE 6 years after LASIK using the
ORBSCAN®
IIz, but the average elevation change observed
here at 6 years means good corneal stability. The ASE was
the most significant prognostic factor in determining if
there will be any changes in the PCE after LASIK.
基金
暂无基金信息
参考文献
1、Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg 1998;14:312-7
2、Binder PS. Analysis of ectasia after laser in situ keratomileusis: risk factors. J Cataract Refract Surg 2007;33:1530-8.
3、Kim TH, Lee D, Lee HI. The safety of 250 microm residual stromal bed in preventing keratectasia after laser in situ keratomileusis (LASIK). J Korean Med Sci 2007;22:142-5.
4、Randleman JB, Russell B, Ward MA, et al. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110:267-75.
5、Twa MD, Nichols JJ, Joslin CE, et al. Characteristics of corneal ectasia after LASIK for myopia. Cornea 2004;23:447-57
6、Pallikaris IG, Kymionis GD, Astyrakakis NI. Corneal ectasia induced by laser in situ keratomileusis. J Cataract Refract Surg 2001;27:1796-802.
7、Martin R, Rachidi H. Stability of posterior corneal elevation one year after myopic laser in situ keratomileusis. Clin Exp Optom 2012;95:177-86.
8、Grewal DS, Brar GS, Grewal SP. Posterior corneal elevation after LASIK with three fl ap techniques as measured by Pentacam. J Refract Surg 2011;27:261-8.
9、Ciolino JB, Belin MW. Changes in the posterior cornea after laser in situ keratomileusis and photorefractive keratectomy. J Cataract Refract Surg 2006;32:1426-31.
10、Miháltz K, Kovács I, Takács A, et al. Evaluation of keratometric, pachymetric, and elevation parameters of keratoconic corneas with pentacam. Cornea 2009;28:976-80.
11、Baek T, Lee K, Kagaya F, et al. Factors affecting the forward shift of posterior corneal surface after laser in situ keratomileusis. Ophthalmology 2001;108:317-20.
12、Miyata K, Tokunaga T, Nakahara M, et al. Residual bed thickness and corneal forward shift after laser in situ keratomileusis. J Cataract Refract Surg 2004;30:1067-72.
13、Ciolino JB, Khachikian SS, Cortese MJ, et al. Longtermstability of the posterior cornea after laser in situ keratomileusis. J Cataract Refract Surg 2007;33:1366-70.
14、Twa MD, Roberts C, Mahmoud AM, et al. Response of the posterior corneal surface to laser in situ keratomileusis for myopia. J Cataract Refract Surg 2005;31:61-71.
15、Grzybowski DM, Roberts CJ, Mahmoud AM, et al. Model for nonectatic increase in posterior corneal elevation after ablative procedures. J Cataract Refract Surg 2005;31:72-81.
16、Randleman JB, Woodward M, Lynn MJ, et al. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology 2008;115:37-50.
17、Quisling S, Sjoberg S, Zimmerman B, et al. Comparison of Pentacam and Orbscan IIz on posterior curvature topography measurements in keratoconus eyes. Ophthalmology 2006;113:1629-32.
18、Hernández-Quintela E, Samapunphong S, Khan BF, et al. Posterior corneal surface changes after refractive surgery. Ophthalmology 2001;108:1415-22.
19、Maloney RK. Discussion of paper by Wang Z, Chen J, Yang G. Posterior corneal surface topographic changes after laser in situ keratomileusis are related to residual corneal bed thickness. Ophthalmology 1999;106:409-10.
20、Cheng AC, Ho T, Lau S, et al. Evaluation of the apparent change in posterior corneal power in eyes with LASIK using Orbscan II with magnifi cation compensation. J Refract Surg 2009;25:221-8.
21、Nishimura R, Negishi K, Saiki M, et al. No forward shifting of posterior corneal surface in eyes undergoing LASIK. Ophthalmology 2007;114:1104-10.
22、Ha BJ, Kim SW, Kim SW, et al. Pentacam and Orbscan II measurements of posterior corneal elevation before and after photorefractive keratectomy. J Refract Surg 2009;25:290-5.
相关文章
Posterior corneal astigmatism modifications after cataract surgery and its role on total corneal astigmatismYe Dai;Xiaoting Ruan;Wei Wang;Xiaoyun Chen;Guangming Jin;Lanhua Wang;Xiaoxun Gu;Bo Qu;Jianping Liu;Xuhua Tan;Enen Zhang;Jun Fu;Lixia Luo;Zhenzhen Liu;Yizhi Liu,Changes in corneal curvature and aberrations after cataract surgeryAmani E. Badawi;Manal Ali Kasem;Tharwat Mokbel;Eman A. Awad,Changes of anterior segment parameters after horizontal rectus muscles recession versus resection