Progress and prospects: the escalating significance of VR technology in the field of ophthalmology
关键词
摘要
全文
HIGHLIGHTS
1.Critical Discoveries and Outcomes
2.Methodological Innovations
3. Prospective Applications and Future Directions
· The exploration of novel paradigms and harnessing the inherent advantages of VR technology to align with the ever-evolving requisites of ophthalmology emerge as imperative endeavors. Just like artificial intelligence in ophthalmology, developing intelligent machines that learn, reason, judge, and make decisions like humans can better serve humans
INTRODUCTION
METHODOLOGY
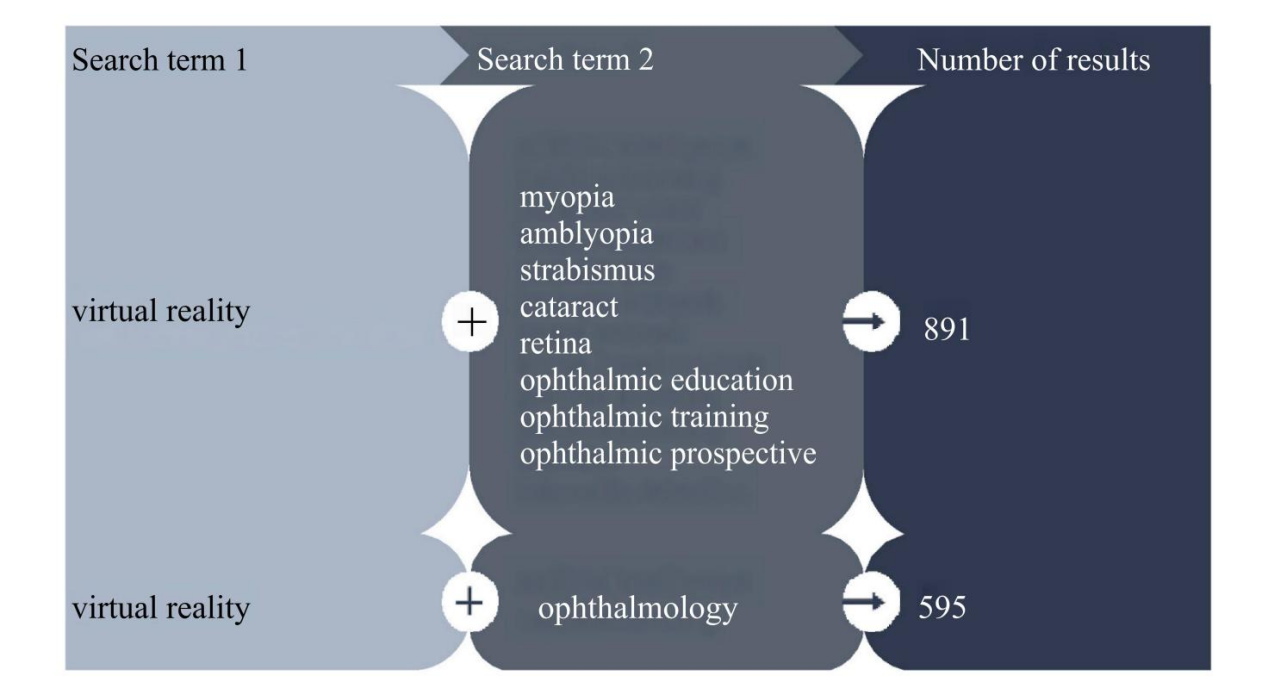
Figure 1 The flowchart of the design of the literature retrieval grid in PubMed and Embase
VR TECHNOLOGY IN OPHTHALMIC DISEASE TREATMENT
Application of VR technology in myopia treatment
Application of VR technology in amblyopia treatment
Table 1 Application of VR technology in amblyopia treatment
|
Authors |
Sample Size |
Purpose |
Results |
|
|
2021 |
Elhusseiny AM et al. [21] |
20 participants |
Evaluation of a prototype virtual reality-based binocular amblyopia treatment for optimal gains in corrected unilateral amblyopia and stereopsis in children and adults aged 7 years and older |
Significant improvement in stereoscopic acuity from 7.3 ± 2 at baseline to 6.6 ± 2.3 at 8 weeks and 6.7 ± 2.6 at 16 weeks |
|
2022 |
Li L et al. [22] |
76 cases of children with amblyopia |
Comparison of the compliance of children with amblyopia trained with the smartphone VR training method (EYEBIT) with those trained with the traditional method |
The EYEBIT method has better adherence than the traditional method. There was a significant correlation between the adherence components of the two methods |
|
2022 |
Tan F et al. [23] |
145 cases of children with amblyopia |
Exploring the potential impact of short-term plastic visual perception training based on VR and AR platforms for people with amblyopia |
Significant improvements in best-corrected visual acuity and fine stereopsis were observed in both the VR and AR groups after training |
|
2021 |
Rajavi Z et al. [17] |
50 cases of unilateral amblyopia in children aged 4 to 10 years |
Comparing the visual effects of masking therapy and VR games for the treatment of amblyopia in children |
Mean best-corrected visual acuity based on logMAR units improved significantly in both groups, with higher changes in BCVA in the VR group than in the masked group |
|
2021 |
Halicka J et al. [24] |
A case of refractive parametric amblyopia in an adult |
Exploring whether adult patients with refractive error and amblyopia improve after VR visual training |
After 1.5 years, the best corrected distance visual acuity of the amblyopic eye improves from 0.05 to 0.5, and the patient gradually develops stereo vision |
|
2020 |
Halika J et al. [25] |
84 cases of refractive parallax amblyopia |
Retrospective analysis of the effectiveness of refractive parametric amblyopia treatment using VR technology in adults with amblyopia |
The best corrected visual acuity improved from 0.48 to 0.58 |
|
2023 |
Molina-Martn A et al. [18] |
4 children |
Exploring the initial experience of using immersive VR devices and prototype software to treat refractive parallax amblyopia |
Visual acuity improved after training, amblyopic eye distance VA improved in all three subjects, final stereo vision was 60 seconds arc, and 3 cpd showed an increase in spatial frequency of approximately 0.5 contrast sensitivity units |
VR: Virtual reality; AR: Augmented reality; BCVA: Best-corrected visual acuity.
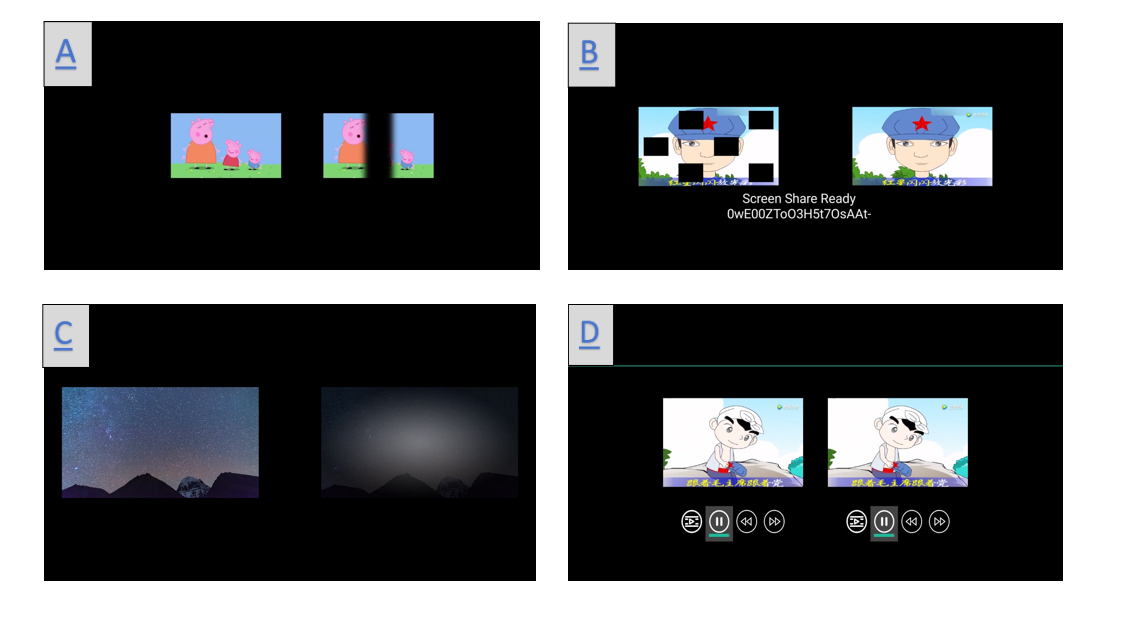
Figure 2 Images of VR technology training amblyopia under different covering conditions.
(A. Strip localized masking mode; B. Multi-region localized masking mode; C. Adjusting contrast sensitivity training mode; D. Fusion training mode under unmasking.)
Application of VR technology in strabismus treatment
Core VR technologies in vision therapy
VR TECHNOLOGY IN OPHTHALMIC EDUCATION
Application of VR technology in the education of ophthalmic students
Ophthalmology student education plays a crucial role in training future professionals in the field. With the increasing complexity of clinical practice and the growing responsibilities of medical care, there is a need for innovative solutions. VR technology has emerged as a promising tool to address these challenges. By utilizing VR technology, students can construct 3D models of eye anatomy and access live-streamed surgeries or recorded videos of VR surgical demonstrations [31]. The visual effects provided by VR are perceptive, realistic, and visible, enabling students to observe and learn more effectively. This immersive learning experience allows students to quickly and intuitively grasp knowledge during the learning process, enhancing their ability to apply it in practice [32].Through immersive visual experiences, students can gain a deeper understanding and analysis of ocular diseases and improve their diagnostic skills. In terms of disease diagnosis [33], the EyesiNet learning platform provides the content that meets the theoretical requirements in the teaching directory. 32 students first learned the theoretical knowledge on the platform and then trained with the Eyesi indirect simulator. After training, it was found that the students' ability to diagnose some retinal diseases has been significantly improved, which can be reflected in the test scores, while the test scores of students without simulator training have not changed [33]. In contrast, the Eyesi indirect simulator can see the real image around the patient's eyes using VR. In this way, the examiner can continue to control his hand under the ophthalmoscope in order to find a stable position for the examination. Through the effective combination of theory and practice, a kind of real and dynamic three-dimensional perception is generated in the mixture of real and virtual situations, which increases students' interest in learning ophthalmology knowledge, which on the one hand improves student learning and on the other hand makes teaching less difficult for teachers. Although there has been a shift in remote learning during the coronavirus disease 2019 (COVID-19) pandemic, starting with pedagogical methods and specific e-learning platforms, this suggests that the importance of virtual learning in ophthalmology has also become more important [34]. VR technology can simulate the real eye surgery scene, provide a more real learning experience, and enable students to receive real-time visual feedback, but it can't completely replace the actual surgery experience and the real patient situation, and the introduction of relevant technologies may have certain technical and financial challenges for schools. Figure 3 mainly shows the application of VR technology in the experimental teaching of ophthalmology. As shown in the figure, in ophthalmology laboratory teaching, we can wear VR glasses to simulate the process of lens production, optometry, so that students are immersed in the hands-on operation, which allows students to quickly understand the content of the experiment and improves learning efficiency.
Figure 3 Application of VR technology in the experimental teaching of ophthalmology
(A. Students' co-participatory VR teaching situation; B. Virtual operation situation of VR teaching and training; C. Eye-hand operation screen in students' VR teaching; D. Simulated eyeglass lens positioning in VR teaching.)

Application of VR technology in the surgery training of ophthalmologists
Table 2 Application of VR technology in cataract surgery training
|
Authors |
Sample Size |
Purpose |
Results |
|
|
2022 |
Nair AG et al. [42] |
35 MSICS Surgeons |
Assessing the facial and content validity of the HelpMeSee cataract surgery simulator |
94.3% of the subjects thought the simulator would help develop hand-eye coordination |
|
2020 |
Ferris JD et al. [43] |
265 trainee surgeons, 17,831 cataract operations |
Study of the impact of the EyeSi surgical simulator on posterior capsular rupture cataract surgery for first- and second-year trainee surgeons |
Complications of posterior capsule rupture cataract surgery fall by 38% for surgeons trained in surgical simulators |
|
2020 |
Adnane I et al. [44] |
12 residents, 300 cataract operations |
Assessing the impact of surgical simulation training on residents |
With the use of the simulator, the average operating time for the surgeon improved by 17 minutes, and only 6.7% of capsular ruptures occurred ruptures occurred |
|
2022 |
Eltanamly RM et al. [45] |
30 ophthalmologists |
Assessing whether virtual reality simulators can help cataract surgeons train their non-dominant hand to perform surgery |
After passing the simulator, 26 surgeons scored 90% of the average score of the dominant hand using the non-dominant hand |
|
2022 |
Mathis T et al. [46] |
24 ophthalmology residents |
Assessing whether the use of the EyeSi simulator improves the time required for cataract training programs for ophthalmology residents |
All doctors completed courses A and B. A total of 22 (91.7%) completed course C, and 5 (20.8%) completed course D |
|
2019 |
Jacobsen MF et al. [47] |
19 Cataract Surgeons |
Exploring the correlation between virtual reality simulator performance and realistic cataract surgery performance |
Pearson correlation of 0.65, with simulator performance significantly correlated with actual cataract surgery performance |
MSICS: Manual small-incision cataract surgery.
Table 3. Differences in Eyesi and Microvistouch technology
|
Eyesi |
Microvistouch |
|
|
Core technology pathways |
Binocular stereo vision is predominant, high hardware dependence, real-time priority |
AI-driven monocular depth estimation with data-driven optimisation and dynamic environment adaptation |
|
Hardware Architecture and Sensor Fusion |
Multi-sensor fusion, high resolution camera |
Lightweight hardware design, IR expandability |
|
Algorithms and Data Processing |
Traditional algorithms combined with deep learning, online calibration techniques |
End-to-end deep learning models, a unified multi-task architecture |
Table 4 Application of VR technology in retinal surgery training
|
Authors |
Sample Size |
Purpose |
Results |
|
|
2022 |
Adatia FA et al. [48] |
22 participants |
Determine whether real-life surgical experience correlates with retinal virtual simulator scores and the impact of various challenges on surgical outcomes |
When comparing Baseline 1 to Baseline 2, the overall improvement in scores reached 12.5% |
|
2022 |
Seddon IA et al. [52] |
10 surgical cases |
Exploring the potential of real-time, three-dimensional surgical monitoring to improve education in vitreoretinal surgery |
Ten surgical cases were successfully transmitted to two surgeons in real time. Case-specific details Visualization of low latency and interaction with the surgical surgeon are possible without compromising the quality of the surgical display |
|
2020 |
Forslund Jacobsen M. et al. [53] |
20 ophthalmologists |
Comparing manual and robotically assisted vitreoretinal surgery using a VR surgical simulator |
Robotic-assisted vitreoretinal surgery can improve precision and reduce tissue damage |
|
2019 |
Ermolaev AP et al. [54] |
19 patients |
Development of a virtual reality device (p-VRD)-based visual field examination method for patients with impaired central vision |
The p-VRD visual field examination evaluates the light sensitivity of non-centrally sighted eyes and is well comparable with the Goldmann test (coefficient of conformity K = 73.7%) |
p-VRD: Virtual reality device; VR: Virtual reality.