A man with asymmetric bilateral choroidal melanocytosis: a case report and literature review
关键词
摘要
全文
HIGHLIGHTS
Pigmentary ocular fundus lesions usually involved in retinal pigment epithelial (RPE) and the choroid. It’s crucial to differentiate between various pigmented fundus lesions, as their nature ranges from benign to malignant and requires different clinical management strategies[1].
Isolated choroidal melanocytosis(ICM) is a rare condition characterized by the flat, discrete, patch choroidal melanotic hyperpigmentation, without ipsilateral iridic or anterior scleral melanocytosis[2–5]. Although choroidal melanocytosis was usually considered a benign condition, several studies have found a close relationship between choroidal melanocytosis and choroidal melanoma[2,4,6–8]. Therefore, an accurate diagnosis of choroidal melanocytosis and its differentiation from other pigmented fundus lesions are essential aspects of clinical practice to mitigate vision-threatening complications and ensure early intervention for potential malignant progression.
In this case, we presented unusual manifestations of bilateral choroidal melanocytosis, along with its defining characteristics through multimodal imaging. To differentiate pigmentary ocular fundus lesions, we summarized the clinical and multimodal imaging features of various diseases.
CASE PRESENTATION
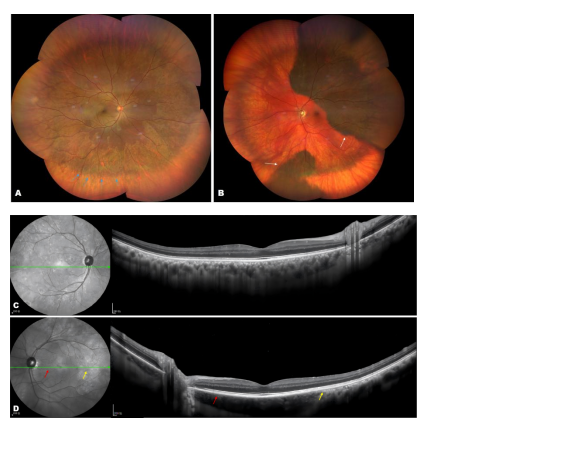
A 60-year-old man of Asian descent presented for regular medical examinations. His best corrected visual acuity was 20/25 OD and 20/25 OS. Slit-lamp examination revealed mild nuclear and cortical cataracts as well as slightly vitreous opacities. The anterior segments shown no other features of ocular melanocytosis. During funduscopic examination, bilateral choroidal melanocytosis with an asymmetry choroidal pigmentation changes was observed. In the right eye, there was diffuse darker coloration from posterior pole to the mid-peripheral retina (Fig 1-A). In the left eye, flat patches of choroidal hyperpigmentation were present, involving the superior and inferior hemisphere regions, while other regions was depigmented (Fig1-B).The margin of hyperpigmentation area on the fundus were indicated by arrow heads in Figure 1.Spectral-domain optical coherence tomography (SD-OCT) revealed normal retinal layers with slightly increased choroidal thickening (Fig 1-C, D). There is no elevation of the retinal pigment epithelium (RPE) or any choroidal mass.Changes in choroidal pigmentation (either an increase or a decrease) led to alterations in OCT findings. Figure 1-D clearly shown an indistinct Sattler’s layer and Haller’s layer at the area of hypopigmentation (red arrow ) and slightly thickened choroid with a distinct structure in the area of hyperpigmentation(yellow arrow).Near infrared reflectance (NIR) images provide a clearer view of mottled focal hyperpigmentation corresponding to the choroidal hyperpigmentation (Fig 1-C, D). The patient denied any ocular history, especially past episodes of uveitis. Additionally, the patient had no other systemic diseases, including dermatological disease such as vitiligo. After a physical examination, no other skin melanocytosis, cutaneous hypopigmentation, or white forelock was found. Based on the medical history, systemic examination, and fundus multimodal imaging, the patient was diagnosed with choroidal melanocytosis with asymmetric fundus manifestations. Although choroidal melanocytosis is typically benign, several studies have identified a potential association between choroidal melanocytosis and choroidal melanoma[4,6,7]. Therefore, the patients requires lifelong follow-up.Figure 1 Multimodal imaging demonstrated bilateral choroidal melanocytosis with asymmetric pigmentation patterns
DISCUSSION
A comprehensive search of the PubMed platform was conducted up to December 20, 2024, using the search terms “choroidal melanocytosis”. The search yielded 15 articles, as shown in Table 1. To date, a total of 100 cases of isolated choroidal melanocytosis have been reported.Although, according to Augsburger et al.,most cases of ICM were unilateral[9], 31 cases of bilateral ICM have been documented. In contrast to our case, these cases with bilateral involvement exhibit symmetrical lesions of ICM[5,10–14].Table 1 Synopsis of cases of isolated choroidal melanocytosis published in Pubmed, 1974–2024
|
Country/Year |
Number of patients |
Gender |
Age
|
Race |
Laterality |
Multimodal imaging findings |
Complications |
Intervention |
|
|
1.Pamela Martin, et al.[5] |
USA/2022 |
1 |
Female |
40 |
Asia |
Bilateral |
FP: Extensive bilateral choroidal melanosis |
- |
Long-term follow-up |
|
2.Arun D Singh, et al. [30] |
Australia/2021 |
22 |
15 males/7 females |
- |
White: 14 cases (64%). Middle Eastern/Asian: 8 cases (36%) |
3 unilateral/ 19bilateral |
FP: Sectoral and temporal CM |
- |
Long-term follow-up |
|
3.Maura Di Nicola, et al.[8] |
USA/2020 |
3 |
- |
- |
White |
Unilateral
|
FP: Darkly pigmented choroidal tumor with prominent overlying lipofuscin and a large associated area of choroidal melanocytosis; AF:Prominent lipofuscin pigment along the posterior margin of the lesion; A-scan and B-scan ultrasonography demonstrated nodular choroidal tumor with low internal reflectivity. |
Developed multifocal uveal melanoma |
Plaque brachytherapy |
|
4.James J Augsburger, et al.[4] |
USA/2020 |
37 |
15 males /22 females |
Mean age: 31.5 years old |
- |
Unilateral in 36 cases; 1 bilateral case with partial iris melanocytosis in the fellow eye |
FP: Homogeneous, flat choroidal hyperpigmentation. B-scan ultrasonography: Flat lesions with no measurable thickness compared to adjacent choroid. Absence of acoustic shadowing or intrinsic vascularity. AF:Absence of lipofuscin/drusen overlying ICM (except in melanoma-associated cases) |
3/37 (8.1%) developed melanoma within ICM; 1/37 (2.7%) had melanoma in the fellow eye |
Plaque radiotherapy |
|
India/2020 |
1 |
- |
- |
Asians |
Bilateral |
FP: Central hypopigmentation with peripheral choroidal hyperpigmentation around the 360° field in both eyes FFA/AF/OCT:NAD |
- |
||
|
6.Amador-Patarroyo et al.[11] |
USA/2019 |
1 |
Female |
50 |
Latin-American |
Bilateral |
FP: Extensive, diffuse, midperipheral hyperpigmentation in an annular pattern, sparing the macula and optic nerve OCT: NAD |
- |
Long-term follow-up |
|
7.Samuel J Fallon, et al.[21] |
USA/2019 |
1 |
Female |
48 |
Caucasian |
Bilateral |
FP: Diffuse bilateral scleral pigmentation and choroidal darkening |
Developed multifocal choroidal melanoma |
Enucleation |
|
8.Kevin D. Heinze, et al.[10] |
USA/2019 |
1 |
Female |
44 |
American Indian |
Bilateral |
FP:Bilateral 360° conffuent annular pattern of isolated choroidal melanocytosis. OCT/AF/ B-scan ultrasonography:NAD |
- |
Long-term follow-up |
|
9.Patricia Hrynchak, et al. [31] |
Canada/2018 |
1 |
Male |
34 |
Greece |
Bilateral |
FP: Large area of flat, confluent choroidal hyperpigmentation with feathered boarders OCT/AF:NAD |
- |
Long-term follow-up |
|
10.Lauren B Mason, et al.[32] |
USA/2016 |
1 |
Female |
24 |
African American |
Bilateral |
OCT:Remarkable for increased choroidal thickness with a normal inner and outer retina. |
- |
Long-term follow-up |
|
11.Marco Pellegrini, et al.[17] |
USA/2014 |
15 |
9 males /6 females |
Mean age 28 years old |
|
|
EDI-OCT: Choroidal melanocytosis shows increased subfoveal choroidal thickness with an apparent increase in the choroidal perivascular stromal tissue and minimal effect on the overlying retina. |
- |
Long-term follow-up |
|
12.Juan P. Velazquez-Martin, et al.[12] |
Canada/2013 |
2 |
- |
- |
White |
Bilateral |
FP: Flat choroidal pigmented lesions FFA/OCT:NAD |
- |
Long-term follow-up |
|
13.Howard F Fine, et al.[14] |
USA/2009 |
1 |
Female |
43 |
White |
FP:Diffuse patchy melanocytic choroidal hyperpigmentation B-scan ultrasonography :NAD |
- |
Long-term follow-up |
|
|
14.T A Kovoor, et al.[13] |
USA/2008 |
1 |
Female |
40 |
Indian |
Bilateral |
choroidal hyperpigmentation with indistinct margins involving most of the posterior pole FFA:NAD |
- |
Long-term follow-up |
|
15.James J Augsburge, et al.[2] |
UK/2006 |
11 |
3 males/7females |
Median age:17 years old |
Caucasian |
Unilateral |
FP:An area of flat choroidal hyperpigmentation |
- |
Long-term follow-up |
In this case, we present unusual manifestations of bilateral choroidal melanocytosis. Choroidal melanocytosis was previously considered part of ocular (dermal) melanocytosis (ODM), a congenital disorder characterized by increased pigmentation involving the periorbital area, episclera, sclera, and choroid[15,16].Ausburger et al first defined choroidal melanocytosis as a distinct clinical entity in 2006 to distinguish clinical characteristics 2 , but it is still poorly recognized and reported. Isolated choroidal melanocytosis presents as sector or partial hyperpigmentation of the choroid, without associated iris or scleral melanocytosis[2,17]. In choroidal melanocytosis, the homogeneously melanotic, completely flat lesions usually located posterior to the equator area[4,18]. According to the study with the largest sample size of choroidal melanocytosis, most cases are considered unilateral2. Only a few cases have reported bilateral choroidal melanocytosis and the pigmentary lesions in both eyes were symmetrical5,19. Bilateral oculodermal melanocytosis is recognized as a risk factor for primary uveal melanoma7.Therefore, for bilateral choroidal melanocytosis with asymmetric pigmentary lesions, we should utilize multimodal imaging techniques to identify the lesions and avoid misdiagnoses. According to previous studies, racial disparities exist in the phenotypic expression of choroidal melanocytosis, particularly regarding variations in choroidal pigmentation and melanoma incidence across ethnic groups. Jae Kyoung Lee et al.,reported a case of ICM with coexistence of choroidal hyperpigmentation and hypopigmentation. They pointed out that there is a higher prevalence of hypopigmented fundi and choroidal melanoma in Caucasian populations compared to Asian demographics, and Asian ICM patients may exhibit phenotypic characteristics analogous to Caucasian pigmentary patterns, suggesting the potential pathological coexistence of choroidal hyperpigmentation and hypopigmentation within individual patients[19].Fundus photography, SD-OCT and NIR are non-invasive techniques suitable for evaluating pigmentary lesions of the retina and choroid. Ultra-widefield fundus photography provides details of peripheral lesions. OCT documents layer-by-layer lesion localization and thickness measurement of choroidal lesions. Shields et al summarized the OCT findings of choroidal melanocytosis, which are characterized by increased subfoveal choroidal thickness, primarily due to thickening of the choroidal perivascular stromal tissue, with minimal impact on the overlying retina[20]. These OCT findings will assist clinicians in distinguishing choroidal melanocytosis from other pigmented choroidal masses with associated elevation, such as choroidal melanocytoma and RPE adenocarcinoma [1,21].Near-infrared reflectance uses light in the near-infrared spectrum, which allows deeper penetration and better visualization of subretinal structures[22].Therefore, NIR enables the detection of outer retinal/choroidal pathologies, especially pigmented lesions[3,23]. In our case, although the OCT findings of the hyperpigmentd area were not very pronounced, NIR imaging was able to clearly delineate the boundaries of the pigment lesions. Other multimodal imaging technigues include fundus autofluorescence(AF), B ultrasonography, fundus fluorescein angiography (FFA), indocyanine green angiography (ICGA) and OCT angiography (OCTA). We summarized the multimodal findings of different pigmentary ocular fundus lesions in Table 2. Recent advancements in the diagnosis and management of choroidal melanocytosis highlight its reliance on multimodal imaging for accurate identification. Key diagnostic modalities include color fundus photography, OCT, and B-scan ultrasonography, which reveal characteristic features such as flat choroidal hyperpigmentation, absence of lipofuscin (in benign cases), and normal retina and choroid layers. While most cases remain asymptomatic and stable, studies report rare malignant transformation (e.g., 8.1% in Augsburger et al., 20204,8,24), necessitating vigilant monitoring. Interventions like plaque brachytherapy are reserved for its most common complication--uveal melanoma. Pathologically, choroidal melanocytosis involves benign proliferation of melanocytes. Current studies advocate for longitudinal surveillance via non-invasive imaging to detect early malignant changes, while molecular research aims to identify biomarkers for risk stratification.
Choroidal melanocytosis should be differentiated from other melanotic retinochoroidal diseases, including: benign and malignant pigmented neoplasms of the retinal pigment epithelium, such as RPE adenoma or adenocarcinoma; benign and malignant pigmented neoplasms of choroid, such as choroidal nevus and melanoma, freckle, and focal aggregates of normal or near-normal uveal melanocytes (FANNUMs); combined hamartoma of the retina and RPE(CHRRPE), congenital hypertrophy of the RPE(CHRPE), RPE hyperplasia, and acquired bilateral patchy-streaky choroidal melanocytic fundopathy associated with cutaneous vitiligo or therapeutic agents[25,1,4,5].Multimodal imaging can provide essential clues for clinicians to make a diagnosis, as shown in Table 2.There are multiple types of discrete melanocytic choroidal lesions, including choroidal nevus, melanoma, FANNUMs, and choroidal melanocytosis. FANNUMs are usually discrete, small, and flat lesions without RPE changes, whereas choroidal nevus usually has distinct or feathery margins with RPE changes, such as atrophy, RPE hyperplasia, and RPE fibrous metaplasia[17,26,21,27]. Multimodal imaging features also provide clues for the transformation of choroidal nevi into melanoma[28,29].Shields proposed the mnemonic “To Find Small Ocular Melanoma Doing Imaging” to describe risk factors for the transformation of choroidal nevus into melanoma: thickness > 2 mm on ultrasound, subretinal fluid on OCT, symptoms (visual acuity 20/50 or worse), orange pigment on AF, acoustic hollowness on ultrasound, and tumor diameter>5 mm on fundus photography[30]. Melanocytoma, melanoma, and RPE adenocarcinoma are solid masses with RPE or choroidal elevation, which can be detected by OCT and ultrasound. Choroidal melanoma, the most common primary intraocular malignancy in adults, appears as pigmented or amelanotic lesions with characteristic orange pigment, subretinal fluid, and serous retinal detachment[21].Key imaging findings of choroidal melenoma include acoustic hollowness on ultrasonography, choroidal thickening with shaggy photoreceptors on OCT, and mottled hyperfluorescence with hypocyanescence on angiography (FA/ICGA)[21]. RPE adenoma shares similar clinical features with melanoma and is usually difficult to diagnosis from suspected choroidal melanoma. RPE adenoma usually grows very slowly and invades the overlying retina layers; thus, it often acquires a retinal feeding artery and draining vein[31]. CHRPE is hypertrophic RPE with melanosomes and photoreceptor atrophy. It shows thinning of the overlying retina, loss of photoreceptors, and moderate relative shadowing of the underlying choroid on OCT26.CHRRPE appears as gray retinal mass with traction and retinal vessel tortuosity[32]. Choroidal vitiligo can appear as asymmetric bilateral choroidal hypopigmentation, which is similar to our case, but dermatologic examination can often reveal cutaneous vitiligo or white forelock among these patients. In our case, the patient has no history of intraocular inflammation, trauma, dermatological disease, or any systemic illnesses. Expect for the fundus pigmented lesions, there were no other ocular abnormality. Therefore, the diagnosis of choroidal melanocytosis was made.
Table 2 Clinical and multimodal imaging features of pigmentary fundus lesions
|
The nature of the lesion |
Pathology
|
Clinical Feature
|
Multimodal imaging features |
Management
|
|||||
|
|
|
|
|
Fundus photography |
OCT |
AF |
FFA/ICGA |
Ultrasound |
|
|
Choroidal Freckle (FANNUM) |
Benign |
Focal aggregate of normal choroidal melanocytes |
Asymptomatic,middle age or older adulthood |
Flat, discrete melanotic choroidal lesion |
Hyper-reflective, posterior shadowing; no elevation |
IsoAF |
- |
Non-elevated |
None |
|
Choroidal nevus |
Benign to Suspect |
Benign uveal melanocytes (nevus cells) |
Asymptomatic |
Pigmented lesion with/without RPE changes /amelanotic;drusen |
Thickened choroid; drusen, retinal pigment epithelium detachment,subretinal fluid(SRF) |
HypoAF (orange pigment hyperAF) |
Hypofluorescent |
<2 mm thick; high/low reflectivity |
Monitoring follow-up |
|
Choroidal Melanoma |
Malignant |
Anaplastic uveal melanocytes (uveal malignant melanoma cells) |
The most common adult primary intraocular malignancy with vision loss, field defects, |
Well demarcated,orange pigment , subretinal fluid, or serous retinal detachment |
Thickened choroid, shaggy photoreceptors, SRF; compressed choriocapillaris |
HyperAF (orange pigment) |
Mottled hyperfluorescence; "hot spots"; hypocyanescent |
Dome/mushroom shape; acoustically hollow |
Plaque brachytherapy,enucleation,sclerouvectomy,immunotherapy |
|
Choroidal melanocytosis |
Benign |
Congenital diffuse proliferation of choroidal melanocytes |
Asymptomatic,associated with iris/skin hyper pigmentation |
Flat,patchy melanotic lesion located at posterior to the equator |
Slightly Choroidal thickening |
IsoAF |
- |
Non-elevated |
Monitoring follow-up |
|
RPE adenoma |
Benign to Suspect |
Neoplastic proliferation of rpe cells forming cords or tubules |
Generally diagnosed,more common in female,no predilection for race |
Deeply pigmented, unilateral, abruptly elevated or dome shaped, with associated feeder arterioles, exudation, and ocular inflammation |
HyperreflectiveRPE elevation |
IsoAF |
Hypofluorescence with late staining |
High reflectivitywith solid mass |
Partial lamellar sclerouvectomy or plaque radiotherapy |
|
CHRPE |
Benign |
Hypertrophic RPE with melanosomes |
Asymptomatic |
Flat, black plaque with lacunae/halo,usually located at midperipheral fundus |
Retinal thinning, subretinal cleft |
Hypoautofluorescent |
|
Non-elevated |
None
|
|
CHRRPE |
Benign |
Gliosis and RPE proliferation Vascular and glial hyperplasia |
Gray retinal mass with traction |
Gray retinal mass with traction,uxtapapillary/macular |
Retinal folds, vitreoretinal traction |
IsoAF |
Late staining on FFA |
Non-elevated or slightly elevated |
Vitrectomy for traction |
CONCLUSION
We presented a rare case characterized by bilateral melanocytic hyperpigmentation with different manifestations, which is prone to be misdiagnosis. Although choroidal melanocytosis usually presents asymptomatically, several studies found a close relationship between choroidal melanocytosis and choroidal melanoma[2].Therefore, the patients with this disorder require lifelong follow-up due to its association with the development of choroidal melanoma[2].Correction Notice
NoneAcknowledgements
NoneAuthor Contributions
(I) Conception and design: Xiaolai Zhou, Yuhong Gan(II) Administrative support: Feng Wen
(III) Provision of study materials or patients: Xiaolai Zhou
(IV) Collection and assembly of data: Yuhong Gan
(V) Data analysis and interpretation: Yuhong Gan
(VI) Manuscript writing: All authors
(VII) Final approval of manuscript: All authors