Choroidal neovascularization as the initial manifestation of multiple evanescent white dot syndrome
阅读量:1184
DOI:doi: 10.3978/j.issn.1000-4432.2016.09.10
发布日期:2024-12-01
作者:
Hamid Saf
展开更多 '%20fill='white'%20fill-opacity='0.01'/%3e%3cmask%20id='mask0_3477_29692'%20style='mask-type:luminance'%20maskUnits='userSpaceOnUse'%20x='0'%20y='0'%20width='16'%20height='16'%3e%3crect%20id='&%23232;&%23146;&%23153;&%23231;&%23137;&%23136;_2'%20x='16'%20width='16'%20height='16'%20transform='rotate(90%2016%200)'%20fill='white'/%3e%3c/mask%3e%3cg%20mask='url(%23mask0_3477_29692)'%3e%3cpath%20id='&%23232;&%23183;&%23175;&%23229;&%23190;&%23132;'%20d='M14%205L8%2011L2%205'%20stroke='%23333333'%20stroke-width='1.5'%20stroke-linecap='round'%20stroke-linejoin='round'/%3e%3c/g%3e%3c/g%3e%3c/svg%3e)
关键词
Idiopathic
choroidal neovascularization (CNV)
multiple evanescent white dot syndrome (MEWDS)
tomography
optical coherence
ff uorescein angiography
摘要
To report the case of a patient who presented with idiopathic choroidal neovascularization (CNV)
as the first sign of multiple evanescent white dot syndrome (MEWDS). A 25-year-old woman presented
with recent onset of decreased vision and metamorphopsia in the right eye. The results of fundoscopic
examination, fluorescein angiography, and optical coherence tomography (OCT) were compatible with a
diagnosis of idiopathic CNV, which was treated with one intravitreal injection of bevacizumab. Five years
later, the patient returned complaining of photopsia and decreased vision in the same eye. The fundoscopic
examination showed typical signs of MEWDS. After 3 months, recurrence of CNV was observed in the same
eye. In conclusion, idiopathic CNV might be the only manifestation of a subclinical occurrence of MEWDS.
In this case, it was followed by a recurrence of MEWDS and subsequent reactivation of CNV.
全文
Introduction
Choroidal neovascularization (CNV) is an abnormal
ingrowth of the choroidal vasculature that penetrates
through Bruch’s membrane into the subretinal space. When
CNV occurs in patients aged up to 50 years, etiologies
such as high myopia, ocular histoplasmosis, trauma, and
inflammatory conditions could be responsible. However, in
younger patients, idiopathic CNV remains the second most
common etiology (1).
Multiple evanescent white dot syndrome (MEWDS) is an acute onset inflammatory disease predominantly affecting the outer retina (2). The disease typically affects young to middle-aged myopic women in the second to fourth decades of life. Patients complain of acute, mostly unilateral, painless loss of vision accompanied by photopsia and central or paracentral scotoma (3). Fundoscopy reveals multiple gray to white dots located at the posterior pole that are later replaced by granular macular pigmentary changes. The disease is self-limiting and patients typically regain their previous visual acuity. Rarely, persistent blind spot enlargement is observed (3). It has been suggested that some cases of idiopathic CNV are secondary to a previous occurrence of MEWDS (4-6).
The present report describes a 25-year-old woman initially diagnosed with idiopathic CNV who developed clinical signs of MEWDS 5 years later. It is believed that CNV was the ff rst observed clinical sign of MEWDS.
CNV was reactivated following the recurrence of MEWDS. Treatment of CNV involved one injection of intravitreal bevacizumab for each occurrence. Rouvas et al. showed that the use of intravitreal ranibizumab (Lucentis; Genentech; USA) resulted in the regression of CNV associated with MEWDS (11).
In conclusion, it is suggested that a subclinical episode of MEWDS could be, in part, responsible for clinically diagnosed idiopathic CNV. This conclusion was drawn from the 5-year follow-up of a patient with presumed idiopathic CNV in which recurrence of MEWDS was observed. Long-term follow-up is recommended to clarify the etiology of some cases of presumed idiopathic CNV.
Multiple evanescent white dot syndrome (MEWDS) is an acute onset inflammatory disease predominantly affecting the outer retina (2). The disease typically affects young to middle-aged myopic women in the second to fourth decades of life. Patients complain of acute, mostly unilateral, painless loss of vision accompanied by photopsia and central or paracentral scotoma (3). Fundoscopy reveals multiple gray to white dots located at the posterior pole that are later replaced by granular macular pigmentary changes. The disease is self-limiting and patients typically regain their previous visual acuity. Rarely, persistent blind spot enlargement is observed (3). It has been suggested that some cases of idiopathic CNV are secondary to a previous occurrence of MEWDS (4-6).
The present report describes a 25-year-old woman initially diagnosed with idiopathic CNV who developed clinical signs of MEWDS 5 years later. It is believed that CNV was the ff rst observed clinical sign of MEWDS.
Case presentation
A 25-year-old woman complaining of recent-onset
decreased vision and metamorphopsia in her right eye was
referred to a retina clinic in April 2009. The patient stated
no pertinent medical or ocular history and no significant
family history. The best corrected visual acuity (BCVA) was
20/30 and 20/20 in the right and left eye, respectively. No
relative afferent pupillary defect was detected. Slit lamp biomicroscopic examination of the right eye revealed no
signs of anterior segment pathology, vitreous inff ammation,
or ocular media opacity.
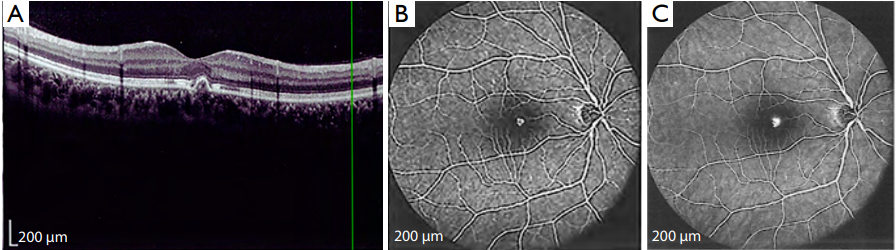
Fundoscopy revealed a small, round, grayish, elevated lesion with indistinct borders located in the juxtafoveal area of the right eye. There were no additional abnormalities affecting the optic disc, retinal vessels, or retinal periphery. Optical coherence tomography (OCT) showed a small amount of subretinal fluid and a focal irregularity of the retinal pigment epithelium layer of the central macula (Figure 1A). Fluorescein angiography demonstrated an early lacy pattern hyperfluorescent spot with late leakage compatible with a juxtafoveal CNV lesion (Figure 1B,C). Results of the ocular examination were unremarkable in the left eye. After a diagnosis of idiopathic CNV was made, the right eye underwent an intravitreal injection of 1.25 mg/0.05 mL bevacizumab (Genentech Inc., San Francisco, CA, USA). At 4 weeks post-injection, the BCVA improved to 20/20 and the metamorphopsia resolved.
Five years later, the patient returned complaining of
deterioration in visual acuity and photopsia in the right
eye. The BCVA was 20/25. Slit lamp examination was
unremarkable. Fundoscopy showed granular lesions within
the macular area with pigmentary changes. OCT showed
only small focal retinal pigment epithelial irregularities
(Figure 2A). Fluorescein angiography revealed multiple
hypofluorescent spots in the early phase with late staining
in the macular region (Figure 2B,C). Indocyanine green
(ICG) angiography disclosed numerous hypofluorescent
spots in the macula and peripapillary region compatible
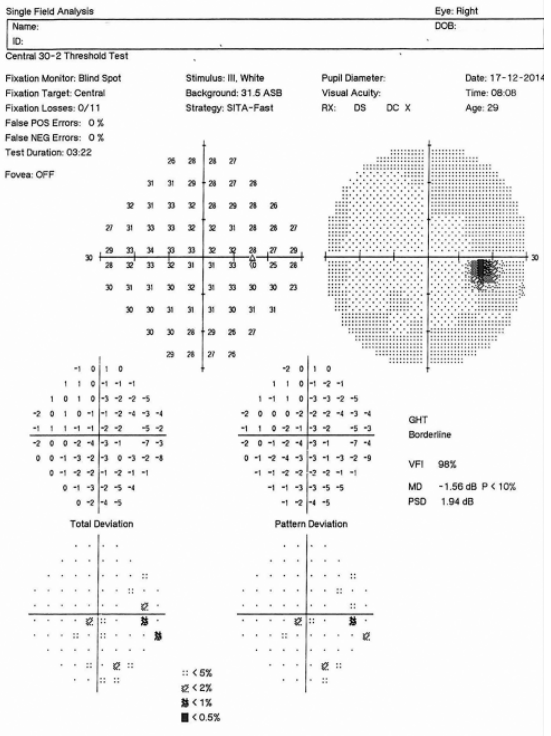
with choriocapillaritis patches (Figure 2D). Automated perimetry (Carl Zeiss Meditec Inc., Dublin, USA) revealed
enlargement of the blind spot (Figure 3). There were no
abnormal findings in the left eye. A diagnosis of MEWDS
was recorded for the right eye.
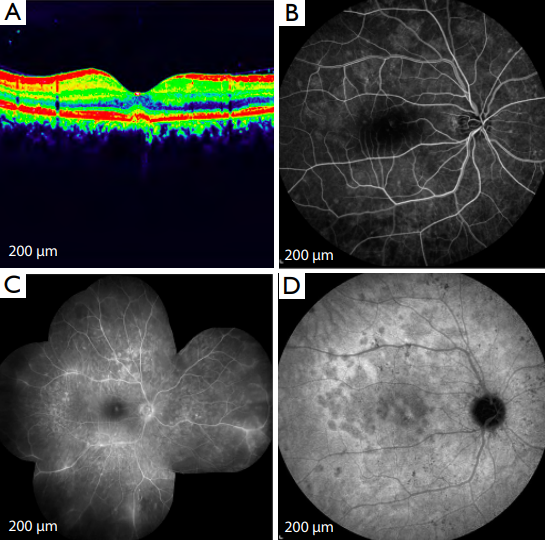 (A) OCT of the right eye shows focal
retinal pigment epithelial irregularities in the central macula as
a typical sign of MEWDS 5 years after the original treatment;
(B) fluorescein angiography of the right eye illustrate multiple
hypoff uorescent spots in the early phase; (C) late staining as a sign
of the MEWDS recurrence; (D) numerous hypofluorescent spots
in the macula and the peripapillary region in the ICG angiography
image at the time of the recurrent attack of MEWDS. CNV,
choroidal neovascularization; MEWDS, multiple evanescent
white dot syndrome; OCT, optical coherence tomography; ICG,
indocyanine green.
(A) OCT of the right eye shows focal
retinal pigment epithelial irregularities in the central macula as
a typical sign of MEWDS 5 years after the original treatment;
(B) fluorescein angiography of the right eye illustrate multiple
hypoff uorescent spots in the early phase; (C) late staining as a sign
of the MEWDS recurrence; (D) numerous hypofluorescent spots
in the macula and the peripapillary region in the ICG angiography
image at the time of the recurrent attack of MEWDS. CNV,
choroidal neovascularization; MEWDS, multiple evanescent
white dot syndrome; OCT, optical coherence tomography; ICG,
indocyanine green.
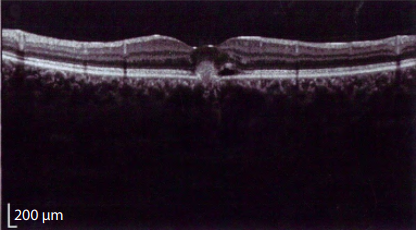
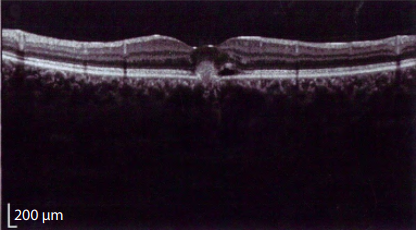
 Three months later, the patient returned with a complaint
of metamorphopsia and vision deterioration in the right
eye. Reactivation of the previous CNV lesion was detected
without further remarkable change in the fundus. OCT
revealed neurosensory detachment (Figure 4). Following
injection of 1.25 mg/0.05 mL intravitreal bevacizumab, the
CNV resolved and the BCVA returned to 20/20.
Three months later, the patient returned with a complaint
of metamorphopsia and vision deterioration in the right
eye. Reactivation of the previous CNV lesion was detected
without further remarkable change in the fundus. OCT
revealed neurosensory detachment (Figure 4). Following
injection of 1.25 mg/0.05 mL intravitreal bevacizumab, the
CNV resolved and the BCVA returned to 20/20.
Fundoscopy revealed a small, round, grayish, elevated lesion with indistinct borders located in the juxtafoveal area of the right eye. There were no additional abnormalities affecting the optic disc, retinal vessels, or retinal periphery. Optical coherence tomography (OCT) showed a small amount of subretinal fluid and a focal irregularity of the retinal pigment epithelium layer of the central macula (Figure 1A). Fluorescein angiography demonstrated an early lacy pattern hyperfluorescent spot with late leakage compatible with a juxtafoveal CNV lesion (Figure 1B,C). Results of the ocular examination were unremarkable in the left eye. After a diagnosis of idiopathic CNV was made, the right eye underwent an intravitreal injection of 1.25 mg/0.05 mL bevacizumab (Genentech Inc., San Francisco, CA, USA). At 4 weeks post-injection, the BCVA improved to 20/20 and the metamorphopsia resolved.
Figure 1 CNV manifestation in the right eye of a 25-year-old woman
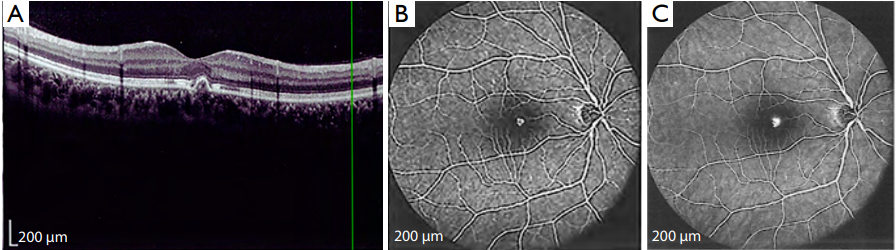
(A) OCT of the right eye shows a small CNV lesion manifesting
as subretinal ff uid and focal irregularity of the central macula; (B) ff uorescein angiography of the right eye demonstrate a hyperff uorescent
lesion with a lacy pattern in the early phase; (C) late leakage of the juxtafoveal CNV lesion. CNV, choroidal neovascularization; OCT,
optical coherence tomography.
Figure 2 Typical presentation of MEWDS in the right eye of a 25-year-old woman.
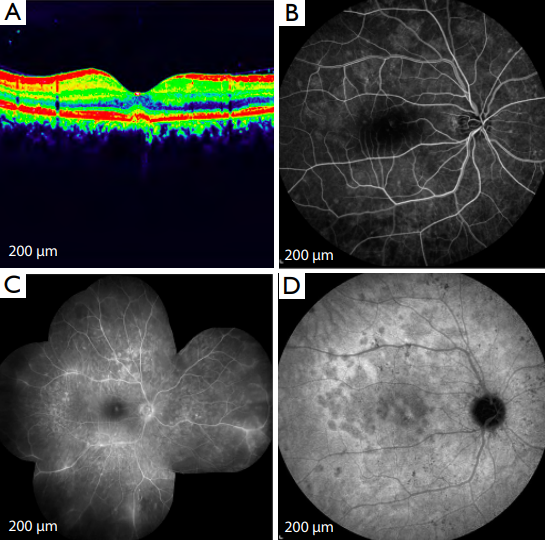
Figure 3 Humphrey visual field test report of the right eye
showing enlargement of the blind spot due to MEWDS attack.
MEWDS, multiple evanescent white dot syndrome.
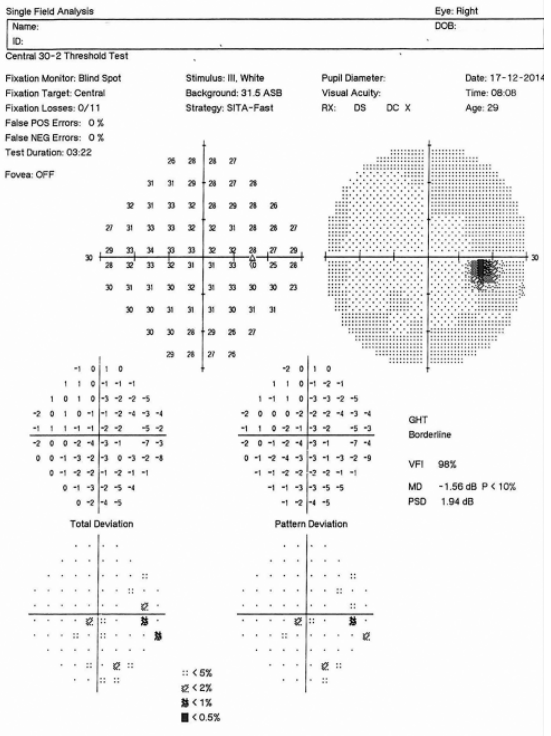
Figure 4 OCT of the right eye showing active CNV lesion with adjacent small neurosensory detachment of the macula 3 months after recurrence of MEWDS. CNV, choroidal neovascularization; MEWDS, multiple evanescent white dot syndrome; OCT, optical coherence tomography.
Discussion
In the current case study, we suggest that idiopathic CNV
may occur following a subclinical episode of MEWDS. The
presumed relationship was confirmed by the occurrence
of a typical attack of MEWDS 5 years after a diagnosis
of idiopathic CNV was made in the same eye. MEWDS
is characterized as a self-limiting monophasic disease for
which recurrence is unusual (2). However, in our patient,
recurrence of MEWDS was observed.
Atypical recurrent forms of MEWDS have been reported in several case studies (6-10). It is interesting to note that the number, laterality, and clinical presentation of the recurrent attacks varied widely among the previous reports. The time between the first episode and its recurrence ranged from 4 months to 9 years. In addition, maintenance therapy with immunosuppressive agents was needed to successfully maintain remission in two cases with multiple uncontrolled outbreaks (5,7). It remains unknown as to why so few cases of MEWDS tend to recur and why different clinical presentations have been described for recurrences of the disease. It is noteworthy that the actual rate of recurrence might be underestimated and that subclinical or atypical attacks could be missed.
The number of MEWDS cases that are complicated by CNV is unknown and their description is confined to a few reports (2,4-12). In the present study, it is believed that idiopathic CNV occurred following an unrecognized subclinical episode of MEWDS, which had resolved by the time of CNV presentation. Therefore, it is advisable to consider MEWDS, particularly in young myopic patients, before making a diagnosis of idiopathic CNV. Machida et al. and Papadia et al. observed comparable cases of presumed idiopathic CNV in which clinical signs of MEWDS manifested only during follow-up examinations (4,5). This finding emphasizes the importance of following patients with idiopathic CNV in order to determine the underlying etiology of the disease.
Atypical recurrent forms of MEWDS have been reported in several case studies (6-10). It is interesting to note that the number, laterality, and clinical presentation of the recurrent attacks varied widely among the previous reports. The time between the first episode and its recurrence ranged from 4 months to 9 years. In addition, maintenance therapy with immunosuppressive agents was needed to successfully maintain remission in two cases with multiple uncontrolled outbreaks (5,7). It remains unknown as to why so few cases of MEWDS tend to recur and why different clinical presentations have been described for recurrences of the disease. It is noteworthy that the actual rate of recurrence might be underestimated and that subclinical or atypical attacks could be missed.
The number of MEWDS cases that are complicated by CNV is unknown and their description is confined to a few reports (2,4-12). In the present study, it is believed that idiopathic CNV occurred following an unrecognized subclinical episode of MEWDS, which had resolved by the time of CNV presentation. Therefore, it is advisable to consider MEWDS, particularly in young myopic patients, before making a diagnosis of idiopathic CNV. Machida et al. and Papadia et al. observed comparable cases of presumed idiopathic CNV in which clinical signs of MEWDS manifested only during follow-up examinations (4,5). This finding emphasizes the importance of following patients with idiopathic CNV in order to determine the underlying etiology of the disease.
CNV was reactivated following the recurrence of MEWDS. Treatment of CNV involved one injection of intravitreal bevacizumab for each occurrence. Rouvas et al. showed that the use of intravitreal ranibizumab (Lucentis; Genentech; USA) resulted in the regression of CNV associated with MEWDS (11).
In conclusion, it is suggested that a subclinical episode of MEWDS could be, in part, responsible for clinically diagnosed idiopathic CNV. This conclusion was drawn from the 5-year follow-up of a patient with presumed idiopathic CNV in which recurrence of MEWDS was observed. Long-term follow-up is recommended to clarify the etiology of some cases of presumed idiopathic CNV.
基金
暂无基金信息
参考文献
1、Cohen SY, Laroche A, Leguen Y, et al. Etiology of choroidal neovascularization in young patients. Ophthalmology 1996;103:1241-4.
2、Marsiglia M, Gallego-Pinazo R, Cunha de Souza E, et al. Expanded clinical spectrum of multiple evanescent white dot syndrome with multimodal imaging. Retina 2016;36:64-74.
3、Quillen DA, Davis JB, Gottlieb JL, et al. The white dot syndromes. Am J Ophthalmol 2004;137:538-50.
4、Machida S, Fujiwara T, Murai K, et al. Idiopathic choroidal neovascularization as an early manifestation of inff ammatory chorioretinal diseases. Retina 2008;28:703-10.
5、Papadia M, Herbort CP. Idiopathic choroidal neovascularisation as the inaugural sign of multiple evanescent white dot syndrome. Middle East Afr J Ophthalmol 2010;17:270-4.
6、Wyhinny GJ, Jackson JL, Jampol LM, et al. Subretinal neovascularization following multiple evanescent whitedot syndrome. Arch Ophthalmol 1990;108:1384-5.
7、Fernández-Barrientos Y, Díaz-Valle D, Méndez-Fernández R, et al. Possible recurrent multiple evanescent white dot syndrome and chroroidal neovascularization. Arch Soc Esp
Oftalmol 2007;82:587-90.
8、Figueroa MS, Ciancas E, Mompean B, et al. Treatment of multiple evanescent white dot syndrome with cyclosporine. Eur J Ophthalmol 2001;11:86-8.
9、Oh KT, Christmas NJ, Russell SR. Late recurrence and choroidal neovascularization in multiple evanescent white dot syndrome. Retina 2001;21:182-4.
10、McCollum CJ, Kimble JA. Peripapillary subretinal neovascularization associated with multiple evanescent white-dot syndrome. Arch Ophthalmol 1992;110:13-4.
11、Rouvas AA, Ladas ID, Papakostas TD, et al. Intravitreal ranibizumab in a patient with choroidal neovascularization secondary to multiple evanescent white dot syndrome. Eur
J Ophthalmol 2007;17:996-9.
12、Callanan D, Gass JD. Multifocal choroiditis and choroidal neovascularization associated with the multiple evanescent white dot and acute idiopathic blind spot enlargement
syndrome. Ophthalmology 1992;99:1678-85.
相关文章
Aiyi Zhou;Chenjing Zhou;Ziyao Liu;Yanlong Quan,Anti-vascular endothelial growth factor treatment for choroidal neovascularization secondary to angioid streaks in pseudoxanthoma elasticum: a case report and systemic review甘雨虹;文峰;周孝来,A man with asymmetric bilateral choroidal melanocytosis: a case report and literature reviewAB033. Implication of beta-adrenergic receptor in choroidal neovascularization