需要与 NTG 鉴别的神经眼科案例分析:病例系列报告和文献回顾
关键词
摘要
全文
文章亮点
1.关键发现
2.已知和发现
3.意义和改变
青光眼是一组以进行性视神经损害为特征的疾病,其病理机制是视网膜神经节细胞的丢失。青光眼性视神经病变的特征性表现为杯盘比(cup-to-disc ratio,C/D)垂直性扩大、颞上方和颞下方视网膜神经纤维层(retinal nerve fiber layer,RNFL)变薄、与之对应的盘沿变窄,并伴有神经纤维束性损害特征的视野缺损[1]。尽管眼压升高是青光眼的主要危险因素,但对于正常眼压性青光眼(normal tension glaucoma, NTG),由于眼压在正常参考值范围内,NTG的诊断需满足青光眼特征性的视神经损害,并排除其他可能导致视神经病变的疾病 [2]。
1 资料与方法
1.1病例1
图1 首次就诊的眼底照相和视野、3个月后的眼底照相
Figure 1 Fundus photograph and visual field at the initial visit, and fundus three months later
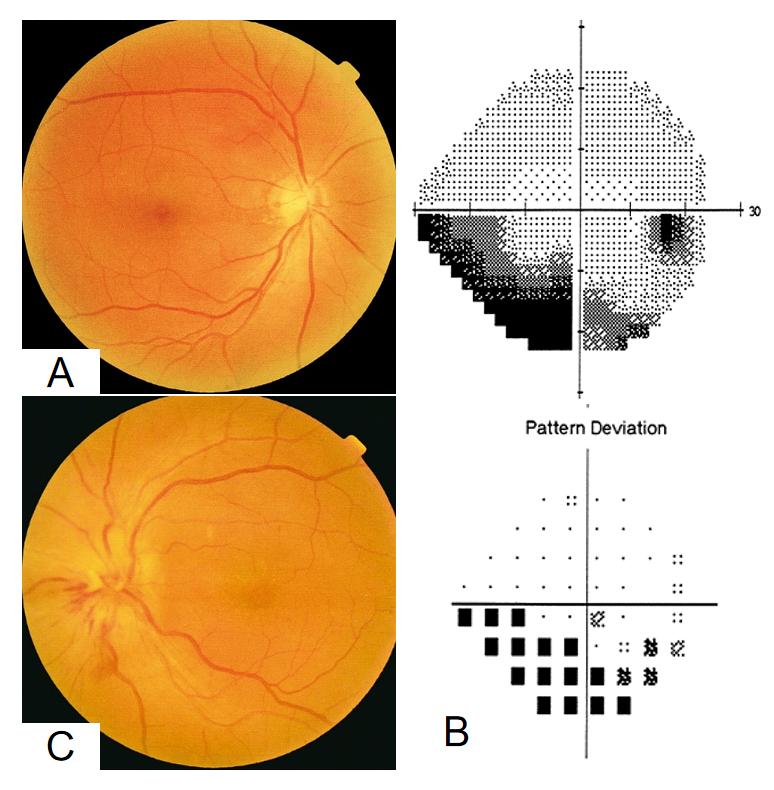
(A) 右眼眼底照相:右眼视盘C/D=0.4,上方盘沿色淡,上方视网膜神经纤维反光消失。(B) 右眼 Humphrey 视野24-2报告:右眼下方与生理盲点相连的弓形暗点,鼻下方损害重。(C) 三个月后左眼眼底彩照:视盘水肿,下方可见放射状出血。
(A) Fundus photograph of right eye: Cup-to-disc ratio 0.4 with pallor of the superior neuroretinal rim and loss of retinal nerve fiber layer reflectance superiorly. (B) Humphrey visual field 24-2 of the right eye: Inferior arcuate scotoma connected to the physiological blind spot, with more severe inferonasally. (C) Fundus photograph of the left eye three months later: Optic disc edema with radial hemorrhages in the inferior.
1.2 病例2
图2 患者首次就诊的眼底照相、OCT和视野检查
Figure 2 Fundus photograph, OCT, and visual field of the initial visit
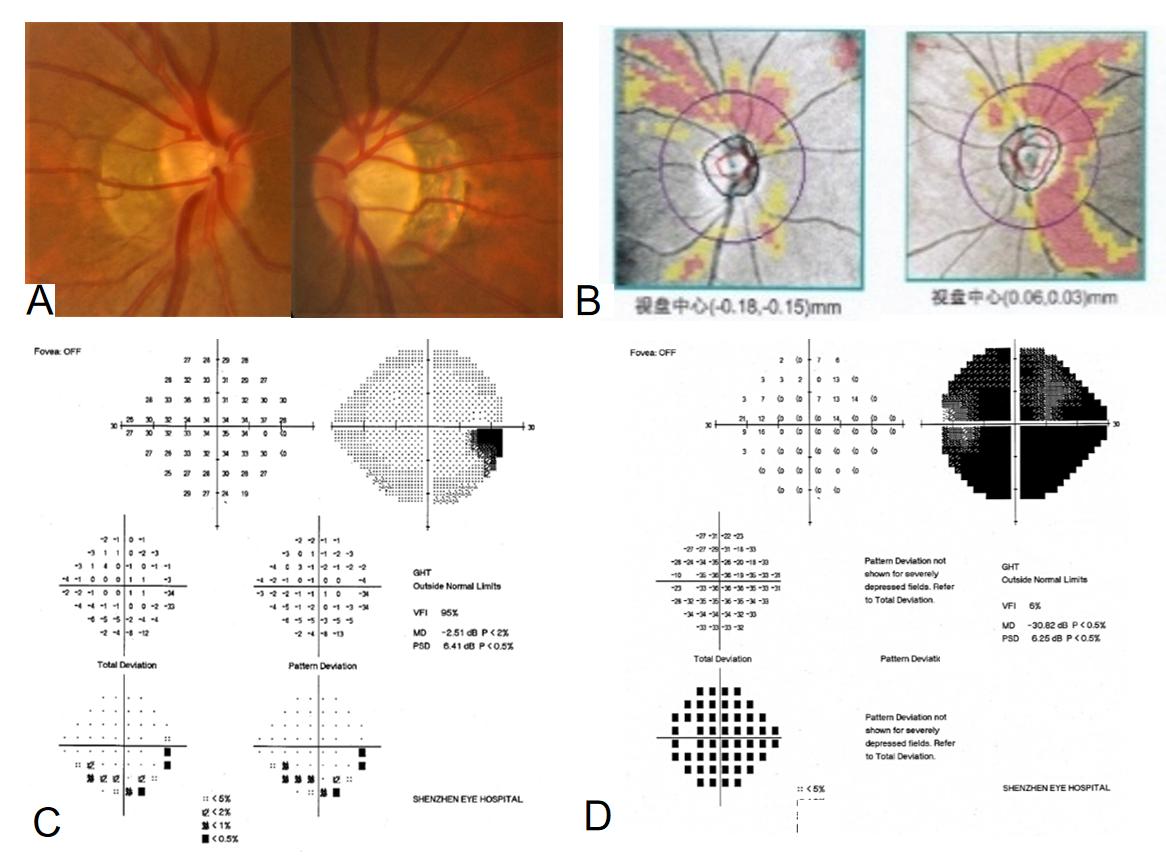
(A) 双眼眼底彩照:双眼视盘周边萎缩弧,右眼视盘色正C/D=0.4,左眼视盘颞侧色淡C/D=0.7。(B) 双眼眼底OCT:右眼颞上方RNFL变薄,左眼颞上和颞下方RNFL变薄。(C) 右眼视野:下方散在暗点。(D) 左眼视野:弥漫性暗点。
(A) Fundus photograph of both eyes: Peripapillary atrophy in both eyes. Optic disc in the right eye showed normal color and C/D of 0.4. Pallor in the temporal optic disc of left eye with a C/D of 0.7. (B) OCT of both eyes: Thinning of the RNFL in the superotemporal quadrant of right eye. Thinning of the RNFL in the superotemporal and inferotemporal quadrants of left eye. (C) Visual field of the right eye: Scattered scotomas in inferior. (D) Visual field of the left eye: Diffuse scotomas.
图3 双眼眼底OCT分析:双眼RNFL厚度相差不大
Figure 3 OCT analysis of bilateral fundus: minimal difference in RNFL thickness between both eyes
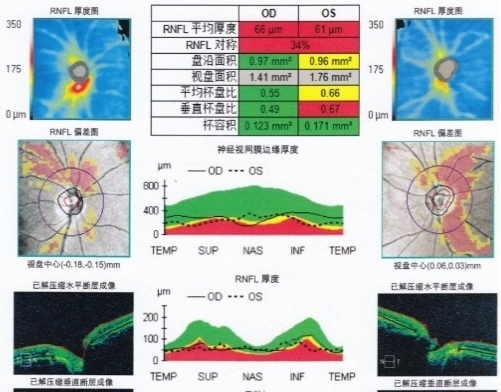
图4 颅脑和眼眶MRI增强序列和病理
Figure 4 Cranial and orbital MRI contrast-enhanced sequences and pathology
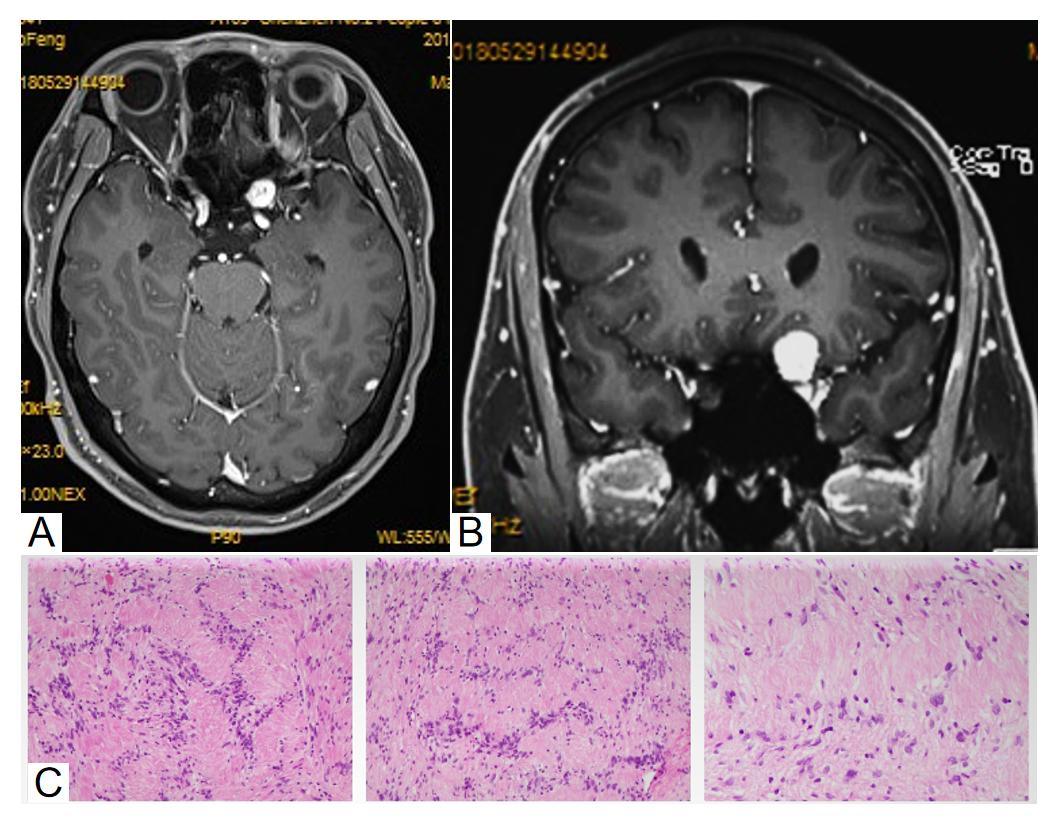
(A)为水平位,(B)为冠状位:左侧前床突区左前缘、视交叉前外侧可见类圆形异常信号灶。(C) 病理检查:肿瘤细胞呈漩涡状排列,胞浆丰富,核卵圆形。
(A) Axial view, (B) coronal view: At the left anterior clinoid region and prechiasmatic lateral area, a roundish abnormal signal focus is visible. (C) Pathological examination: The tumor cells exhibit a whorled growth pattern, with abundant cytoplasm and oval nuclei.
1.3 病例3
图5 患者眼底照相、OCT、视野和基因检测报告
Figure 5 Fundus photography, OCT, visual field, and genetic test results of the patient
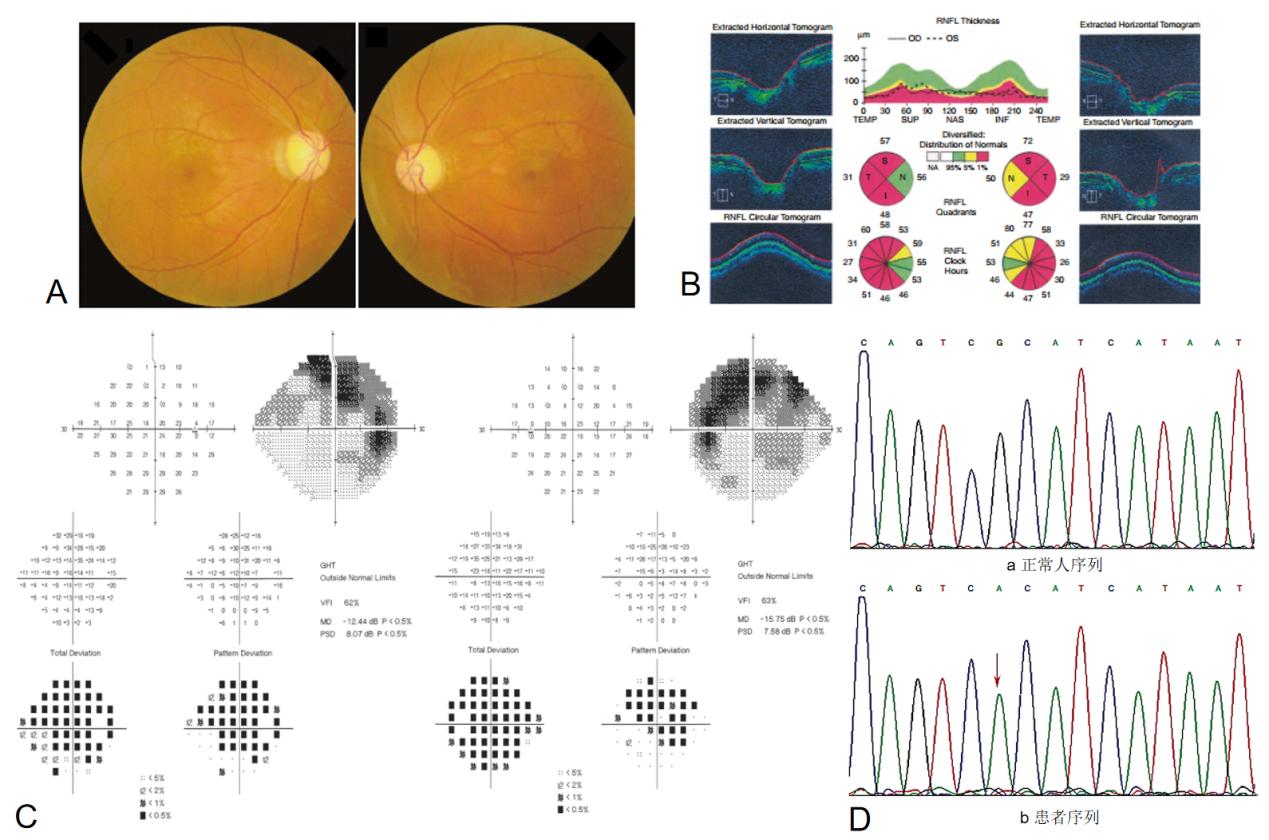
(A) Fundus photograph: Enlarged cup-to-disc ratio in both eyes with temporal pallor and RNFL defects in the temporal, superotemporal, and inferotemporal sectors. (B) OCT: Significant thinning of the RNFL in the temporal papillomacular bundle of both eyes. (C) Visual field: Superior visual field defects in both eyes, crossing the horizontal midline and involving the inferior field. (D) Genetic testing: a Normal sequence, b Patient sequence showing a mutation at nucleotide position 11778 (indicated by red arrow): G→A base substitution.
2 讨论
表1 NTG与常见非青光眼性视神经病变的鉴别要点
Table 1 Key diagnostic points for differentiating NTG from common non-glaucomatous optic neuropathies
|
NTG |
AION |
视神经占位 |
LHON |
|
|
家族史 |
部分有家族史 |
无 |
无 |
母系遗传 |
|
性别 |
无明显差异 |
无明显差异 |
无明显差异 |
青少年男性多见 |
|
眼别 |
双眼发病,病情程度可不一致 |
单眼多见 |
单眼多见 |
双眼多见 |
|
视力 |
早期正常,晚期缓慢下降 |
急性下降 |
进行性视力下降 |
永久性、严重性下降 |
|
眼压 |
正常 |
正常 |
正常 |
正常 |
|
RAPD |
早期阴性,双眼病情不一致可能阳性 |
阳性 |
可能阳性 |
双眼病情不对称时可能阳性 |
|
视盘形态 |
杯盘比垂直性增大,伴有RNFL缺损、盘沿变窄 |
急性期视盘苍白水肿,后期视盘苍白、 |
早期水肿,晚期萎缩 |
急性期视盘充血、神经纤维水肿,后期遗留视神经苍白,颞侧多见,神经纤维变薄 |
|
视野缺损模式 |
神经纤维束性视野缺损,鼻侧阶梯、弓形暗点、环形暗点等 |
水平缺损 |
不规则缺损,与受压部位相关 |
中心暗点 |
|
影像学表现 |
OCT提示RNFL变薄,颅脑和眼眶MRI/CT未见异常 |
眼眶或视神经MRI/CT未见异常 |
颅脑或眼眶MRI/CT可见占位,如增粗、强化或邻近结构受压 |
部分患者MRI可见视交叉的“眼罩征“
|
|
危险因素 |
血管调节能力异常、偏头痛、低血压等 |
高血压、糖尿病、小视杯 |
肿瘤病史、甲状腺眼病、颅内压增高 |
男性、吸烟、饮酒、线粒体突变携带者 |
NTG:正常眼压性青光眼;AION:前部缺血性视神经病变;LHON:Leber遗传性视神经病变;RAPD: 相对性传入性瞳孔障碍;OCT:光学相干断层扫描技术;RNFL:视网膜神经纤维层。
NTG: Normal-Tension Glaucoma; AION: Anterior Ischemic Optic Neuropathy; LHON: Leber's Hereditary Optic Neuropathy; RAPD: Relative Afferent Pupillary Defect; OCT: Optical Coherence Tomography; RNFL: Retinal Nerve Fiber Layer.